Sleep Apnea Specialist Singapore: Diagnosis and Treatment Options
Does your partner frequently wake you up because you’ve stopped breathing during sleep? Sleep apnea causes breathing to repeatedly stop and start during sleep, with pauses lasting from seconds to minutes. The condition manifests in three forms: obstructive sleep apnea (OSA) where throat muscles relax and block airways, central sleep apnea where the brain fails to signal breathing muscles properly, and complex sleep apnea syndrome combining both types. OSA accounts for most cases and responds to various ENT interventions guided by a sleep apnea specialist Singapore.
Untreated sleep apnea leads to fragmented sleep patterns that prevent proper rest cycles, causing daytime fatigue that impairs concentration, decision-making, and reaction times. The repeated oxygen drops strain the cardiovascular system, increasing blood pressure and heart rhythm irregularities. Patients may remain undiagnosed because they attribute symptoms to stress or aging, unaware that snoring and gasping episodes signal a treatable medical condition requiring evaluation by a healthcare professional through ENT clinics.
Table of Contents
Recognizing Sleep Apnea Symptoms
Loud, chronic snoring differs from occasional snoring through its consistency and volume, often disturbing bed partners nightly. The snoring pattern includes periods of silence followed by choking or gasping sounds as breathing resumes. Partners frequently report watching their loved one stop breathing for concerning periods before suddenly gasping for air.
Morning symptoms extend beyond typical grogginess. Patients wake with dry mouth from breathing through their mouth all night, plus headaches from oxygen deprivation and blood pressure fluctuations. The throat feels sore and scratchy despite no signs of infection. These symptoms improve within an hour of waking but return each morning.
Daytime effects accumulate progressively. Concentration problems manifest as difficulty completing tasks that previously required minimal effort. Memory lapses become frequent, with patients forgetting appointments, conversations, or where they placed items. Irritability and mood changes strain relationships as exhaustion affects emotional regulation. Some patients fall asleep during meetings, while driving, or mid-conversation.
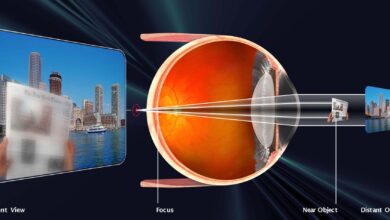
Physical examination findings include enlarged tonsils, elongated soft palate, or a tongue that sits high in the mouth. Larger neck circumference correlates with increased OSA risk. Retrognathia, where the lower jaw sits further back than normal, narrows the airway space. Nasal obstruction from deviated septum or enlarged turbinates forces mouth breathing that worsens collapse.
Diagnostic Testing Methods
Polysomnography is a commonly used method for sleep apnea diagnosis, recording brain waves, oxygen levels, heart rate, and breathing patterns during overnight observation. The test measures the Apnea-Hypopnea Index (AHI), counting breathing interruptions per hour: mild OSA shows several events, moderate shows more frequent events, and severe shows the most frequent events per hour. Oxygen saturation drops below normal levels indicate significant disruption requiring intervention.
Home sleep tests offer convenience for straightforward cases, using portable devices that measure breathing patterns, oxygen levels, and heart rate. Patients wear a finger oxygen sensor, chest belt to detect breathing effort, and nasal cannula to monitor airflow. The simplified testing works well for suspected moderate to severe OSA without other sleep disorders. Results help determine if comprehensive lab testing is necessary.
Drug-induced sleep endoscopy (DISE) allows ENT specialists to visualize airway collapse patterns while patients sleep under light sedation. A flexible endoscope inserted through the nose shows where obstruction occurs – whether at the soft palate, tongue base, lateral walls, or epiglottis level. This dynamic assessment guides surgical planning by identifying anatomical targets.
Imaging studies complement clinical findings. Lateral cephalometry X-rays measure skeletal relationships and soft tissue dimensions. CT scans reveal sinus disease, nasal polyps, or turbinate hypertrophy contributing to obstruction. MRI evaluates soft tissue volumes and tongue fat content that narrow airways.
CPAP Therapy and Alternatives
Continuous Positive Airway Pressure (CPAP) delivers pressurized air through a mask, creating an air splint that prevents airway collapse. Current machines automatically adjust pressure throughout the night based on detected events. Heated humidification reduces nasal dryness and congestion that cause many patients to abandon therapy. Mask options include:
- Nasal pillows for minimal contact
- Nasal masks covering the nose only
- Full-face masks for mouth breathers
CPAP compliance requires adjustment periods. Initial difficulties include:
- Mask discomfort
- Claustrophobia
- Air leaks
- Pressure intolerance
Gradual pressure ramping helps patients fall asleep before therapeutic levels engage. Mask fitting sessions ensure proper seal without excessive tightness. Regular filter changes and daily cleaning prevent infections and maintain optimal function.
Oral appliances offer CPAP alternatives for mild to moderate OSA. Mandibular advancement devices pull the lower jaw forward, increasing airway space behind the tongue. Tongue retaining devices hold the tongue forward using gentle suction. Custom-fitted devices from dental specialists provide better comfort and effectiveness than over-the-counter options. Regular adjustments optimize positioning while monitoring for jaw discomfort or bite changes.
Positional therapy benefits patients whose OSA occurs primarily when sleeping supine. Tennis balls sewn into pajama backs provide basic position training. Electronic position monitors vibrate when detecting back sleeping, prompting position changes without full awakening. Wedge pillows and adjustable beds maintain head elevation that reduces airway collapse.
Surgical Treatment Options
Uvulopalatopharyngoplasty (UPPP) removes excess tissue from the soft palate, uvula, and pharynx to widen the airway. The procedure addresses retropalatal obstruction identified during examination or DISE. Modified techniques preserve muscle function while removing obstructive tissue. Recovery involves two weeks of significant throat pain managed with medications and a soft diet.
Nasal surgeries correct structural problems forcing mouth breathing. Septoplasty straightens deviated septums blocking airflow. Turbinate reduction shrinks enlarged structures using radiofrequency, laser, or surgical trimming. Functional endoscopic sinus surgery opens blocked sinuses causing chronic congestion. Combined procedures address multiple obstruction sites during single operations.
Did You Know?
The genioglossus muscle, which forms the bulk of your tongue, plays an important role in maintaining airway patency during sleep. When this muscle loses tone during REM sleep, the tongue can fall backward and obstruct breathing, which is why many sleep apnea surgical procedures focus on repositioning or advancing tongue attachment points.
Tongue base procedures target obstruction behind the tongue. Genioglossus advancement pulls the tongue muscle attachment forward by repositioning a small window of chin bone. Hyoid suspension lifts and stabilizes the hyoid bone that anchors tongue muscles. Tongue reduction using radiofrequency or surgical techniques decreases tissue volume in selected cases.
Maxillomandibular advancement (MMA) represents a surgical option for severe OSA, moving both upper and lower jaws forward to enlarge the entire airway. The procedure requires careful planning with orthodontic preparation and post-operative orthodontics to maintain proper bite relationships. Recovery extends several weeks with initial jaw wiring or elastic fixation.
Hypoglossal nerve stimulation implants offer treatment for moderate to severe OSA patients failing CPAP therapy. The device monitors breathing patterns and stimulates the hypoglossal nerve during inspiration, moving the tongue forward to maintain airway patency. Patients control therapy using handheld remotes, with many achieving significant AHI reductions.
Lifestyle Modifications and Management
Weight reduction through caloric restriction and exercise decreases neck fat deposits and tongue volume that narrow airways. Weight loss improves AHI scores and reduces CPAP pressure requirements. Bariatric surgery provides improvements for severely obese patients, though OSA may persist requiring continued treatment.
Alcohol cessation eliminates a major OSA trigger. Alcohol relaxes throat muscles excessively and delays arousal responses to breathing interruptions. Evening alcohol consumption particularly worsens sleep apnea severity. Similarly, sedative medications including benzodiazepines and muscle relaxants increase airway collapse risk.
Sleep positioning strategies maximize airway patency. Side sleeping reduces tongue and palate collapse compared to supine positions. Head elevation using wedge pillows or adjustable beds decreases fluid accumulation in neck tissues. Avoiding sleep deprivation helps maintain muscle tone that keeps airways open.
Important Note
Driving while experiencing untreated sleep apnea increases accident risk comparable to alcohol impairment. The Land Transport Authority requires drivers with moderate to severe OSA to demonstrate successful treatment compliance before license renewal.
Nasal breathing optimization improves sleep quality and treatment success. Saline rinses clear mucus and allergens causing congestion. Nasal strips or dilators increase airflow mechanically. Treating allergic rhinitis with antihistamines or nasal steroids reduces inflammation blocking airways.
What Our ENT Specialist Says
ENT evaluation extends beyond identifying anatomical obstruction sites. We assess how multiple factors interact – examining not just tonsil size but how the tongue sits, how the palate moves, and how nasal breathing affects overall airway dynamics. Many patients benefit from combination approaches rather than single interventions.
Surgical success depends heavily on proper patient selection and realistic expectations. DISE findings guide our recommendations by showing exactly what happens during sleep rather than relying solely on awake examinations. Some patients achieve complete resolution while others see meaningful improvements that make CPAP therapy more tolerable.
Treatment plans evolve based on response monitoring. Initial CPAP trials may reveal pressure requirements suggesting specific anatomical corrections. Post-surgical sleep studies determine if additional interventions would provide benefit. Regular follow-up ensures long-term success as aging and weight changes affect airway dynamics.
Putting This Into Practice
- Consider scheduling a sleep study if your partner reports loud snoring with breathing pauses, or if you experience unexplained daytime fatigue despite adequate sleep hours. Document symptoms including morning headaches, concentration difficulties, and mood changes to discuss during consultation.
- Track your sleep patterns using smartphone apps or wearable devices that monitor sleep duration, interruptions, and snoring episodes. Note factors that worsen symptoms like alcohol consumption, sleeping position, or weight changes.
- Consider conservative measures while awaiting specialist evaluation: sleep on your side using body pillows for support, elevate your head with wedge pillows, and establish consistent sleep schedules allowing adequate rest time.
- Prepare for appointments by listing all medications including supplements, previous surgeries especially involving the nose or throat, and family history of sleep disorders or cardiovascular disease.
- Involve your bed partner in consultations as they provide valuable observations about breathing patterns, snoring characteristics, and behavioral changes you may not recognize.
When to Seek Professional Help
- Loud snoring that disturbs others nightly
- Witnessed breathing pauses during sleep
- Gasping or choking episodes that wake you
- Morning headaches occurring several times weekly
- Excessive daytime sleepiness affecting work performance
- Falling asleep while driving or during conversations
- High blood pressure resistant to medications
- Heart rhythm irregularities without clear cause
- Difficulty concentrating despite adequate sleep
- Memory problems affecting daily activities
Commonly Asked Questions
How long does sleep apnea diagnosis take?
Initial consultation and examination require one visit, followed by overnight sleep study scheduling within two to four weeks. Results interpretation and treatment planning occur during a follow-up appointment one week after testing. Home sleep tests provide results, typically within three to five days.
Can children develop sleep apnea?
Pediatric sleep apnea commonly results from enlarged tonsils and adenoids blocking airways. Symptoms include snoring, mouth breathing, bedwetting, and behavioral problems. Adenotonsillectomy may address most pediatric cases, though some children require orthodontic intervention for jaw abnormalities.
Does sleep apnea worsen with age?
Muscle tone naturally decreases with aging, increasing airway collapse tendency. Post-menopausal hormonal changes affect fat distribution and muscle strength. However, treatment remains effective regardless of age, with many older patients experiencing quality of life improvements.
What happens if CPAP doesn’t work?
CPAP intolerance affects many patients initially, but issues often resolve with mask adjustments, pressure modifications, or comfort features. Alternative treatments include oral appliances, positional therapy, or surgical options. Combination approaches often succeed where single treatments fail.
Can sleep apnea return after surgery?
Weight gain, aging, and tissue changes can cause symptom recurrence years after surgery. Regular monitoring with periodic sleep studies ensures early detection of returning problems. Additional procedures or non-surgical treatments may help maintain long-term control.
Next Steps
Proper sleep apnea evaluation identifies the most effective treatment approach for your specific condition. CPAP therapy works for most patients, while surgical options address anatomical obstructions when conservative treatments prove inadequate. Combination approaches often provide optimal long-term control.
If you’re experiencing loud snoring with breathing pauses, excessive daytime fatigue, or morning headaches, consult an ENT specialist for comprehensive sleep apnea evaluation and treatment planning.