Food intolerances can be frustrating and debilitating for many people. Unlike food allergies, which trigger an immediate immune system response, food intolerances cause more gradual and varied symptoms that can be difficult to link back to a particular food or ingredient. However, research increasingly shows that many common food intolerances may actually have an autoimmune component.
Table of Contents
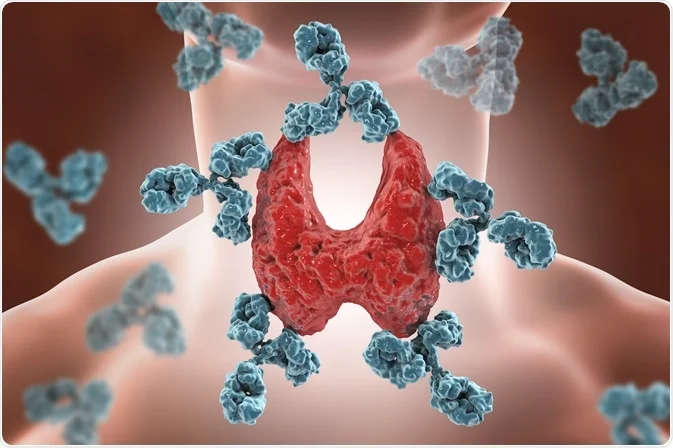
How Autoimmune Disorders Work
Autoimmune diseases occur when the body’s immune system mistakenly attacks healthy cells or tissues. In autoimmune forms of food intolerance, the immune system generates antibodies that react to particular foods and trigger symptoms.
One of the most common autoimmune food intolerances is coeliac disease, which is estimated to affect 1 in 100 people in the UK. In coeliac disease, the immune system reacts to gluten, a protein found in grains like wheat, barley and rye. Eating gluten triggers inflammation and damage to the small intestines, leading to digestive issues, malnutrition and other problems. The only treatment for coeliac disease is adhering to a strict gluten-free diet. If you are suffering from coeliac disease, a coeliac coach can help you manage your diet. For example, Ali Walsh, a gluten-free coach, makes living a life without gluten less stressful.
Other Food Intolerances
While coeliac disease is one of the most prevalent and best understood autoimmune food reactions, researchers believe there are likely many others that have not been fully identified and described.
For example, some cases of non-coeliac gluten sensitivity may involve an autoimmune reaction to gluten. There is also evidence linking autoimmunity to other common food intolerances like dairy, soy, eggs, and corn.
Autoimmune reactions can develop when the gut barrier becomes overly permeable or “leaky”, allowing food proteins to enter the bloodstream, which triggers the immune system to produce antibodies against those foods.
The Symptoms of Food Tolerances
Identifying autoimmune food intolerances can be tricky since the symptoms are often delayed and non-specific. Symptoms may include bloating, abdominal discomfort, fatigue, headaches, brain fog, skin problems, joint pain, diarrhoea or constipation. Lab tests like blood antibody tests can sometimes help identify suspected autoimmune triggers.
The most definitive way to diagnose an autoimmune food reaction is with an elimination diet, where the suspected trigger food is removed from the diet for several weeks, and then carefully reintroduced while monitoring symptoms.
Managing Food Intolerances
Managing autoimmune forms of food intolerance focuses on avoiding the trigger food. For conditions like coeliac disease, this means strict lifelong avoidance of gluten. Following an elimination diet under the supervision of a dietitian can help identify problem foods. Reading food labels carefully and being aware of hidden sources of problem ingredients in foods is also essential.
In some cases, nutritional supplements may be needed to correct deficiencies caused by chronic inflammation and intestinal damage. Paying close attention to symptoms and flare-ups can help determine if accidental exposures are occurring.
While autoimmune food intolerances can be challenging, a better understanding of the role the immune system plays in these conditions provides new opportunities for improved diagnosis and management. Increasing awareness of autoimmune mechanisms may help many people who struggle with unexplained food intolerances finally get answers and relief.
Going forward, further research into autoimmune forms of food intolerance promises to elucidate the complex links between diet, immunity and health.